
Additional imaging was done if a patient's condition worsened. Computed tomographic scans were done for all of the patients on admission and before initiation of AC. Severe systemic bleeding was defined as any gastrointestinal tract, intra-abdominal, or external bleeding necessitating transfusion. Outcome measures and adverse events were captured prospectively. The decisions of whether to bridge and whether to use heparin or low-molecular-weight heparin were made based on clinical judgment and personal preference of the treating physician. In patients deemed candidates for AC, warfarin treatment is started in the hospital.
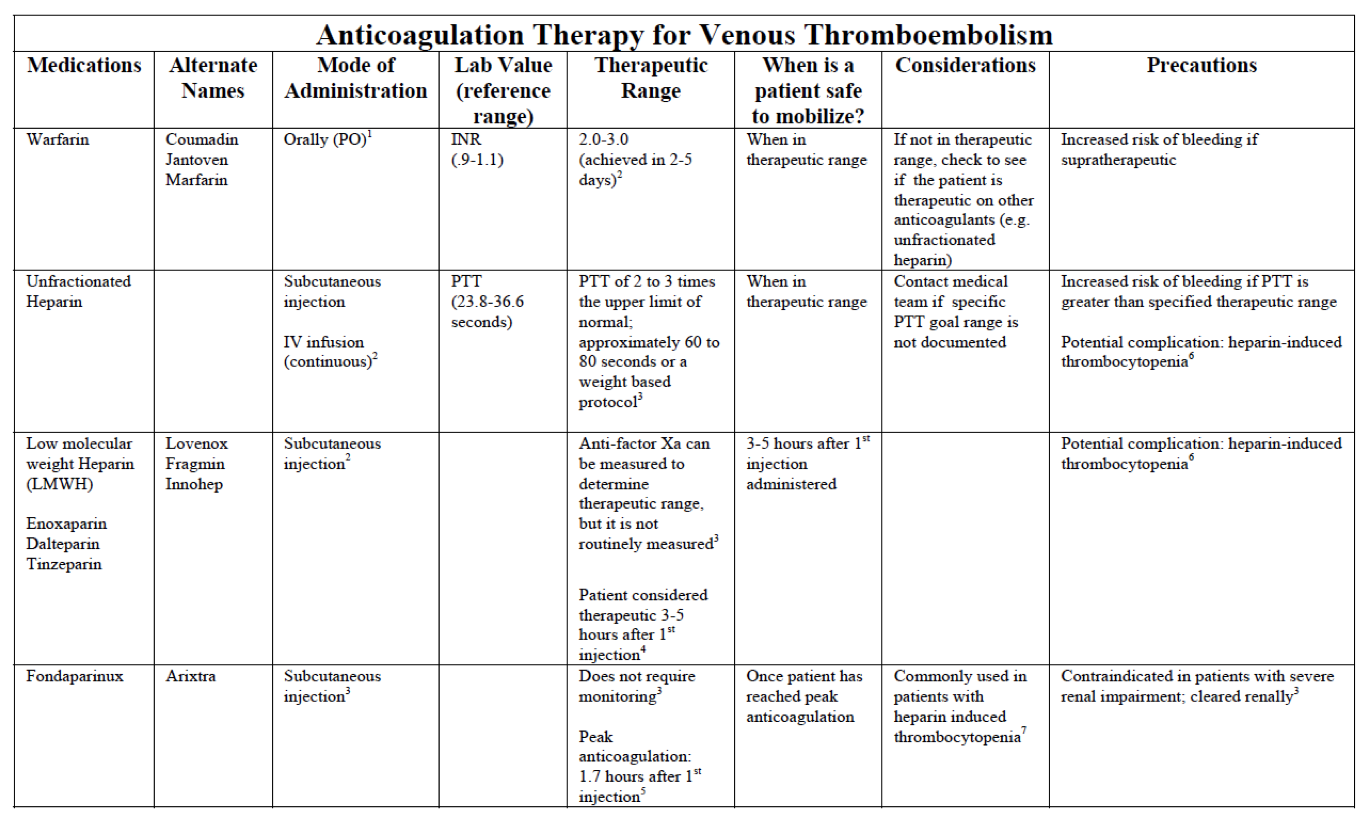
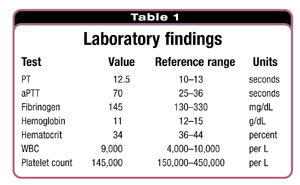
As a general rule, in patients with large infarcts who were debilitated, there is an inclination to defer the decision of AC until the patient is stabilized. All of the patients were cared for by the same stroke team. Patients receiving thrombolytic therapy were excluded. A cardioembolic cause was diagnosed when the patient had 1 of the following: atrial fibrillation (by history or electrocardiography), mechanical heart valve, significant rheumatic valvular disease, severe focal cardiac wall motion abnormalities (in the absence of significant ipsilateral carotid atherosclerosis) or a cardiac clot visualized on an echocardiogram, and patent foramen ovale in the presence of venous thrombosis and in the absence of significant atherosclerosis. We conducted a retrospective review of all patients admitted to our stroke center who were diagnosed with CES from April 1, 2004, to June 30, 2006, and not treated with tissue plasminogen activator. Our aim was to compare these AC strategies, focusing on efficacy in preventing early stroke recurrence, risk of serious bleeding, functional outcome, and mortality. Because warfarin sodium takes several days to reach a therapeutic international normalized ratio (INR), 3 strategies are used during that period: warfarin alone or with aspirin (no bridging) intravenous heparin sodium combined with warfarin (heparin bridging ) and full-dose enoxaparin sodium (a low-molecular-weight heparin) combined with warfarin (enoxaparin bridging ). There is no consensus on the best way to initiate AC after CES. 3, 4 Nevertheless, most patients with CES ultimately need AC. 2 Current guidelines do not support the routine anticoagulation (AC) of patients with CES in the acute phase. 1 In addition, cardioembolic stroke (CES) carries increased risk of hemorrhagic transformation (HT). The infarct is typically larger than that in atherothrombotic stroke and the outcome is poorer. Published online J(doi:10.1001/archneur.65.9.noc70105).Ĭardioembolism accounts for 20% of ischemic strokes. Heparin bridging and enoxaparin bridging increase the risk for serious bleeding. Systemic bleeding occurred in 2 patients (1%) and was associated with heparin bridging ( P = .04).Ĭonclusions Anticoagulation of patients with cardioembolic stroke can be safely started with warfarin shortly after stroke. All of the symptomatic hemorrhagic transformation cases were in the enoxaparin bridging group (10%) ( P = .003). Hemorrhagic transformation occurred in a bimodal distribution-an early benign hemorrhagic transformation and a late symptomatic hemorrhagic transformation. Progressive stroke was the most frequent serious adverse event, seen in 11 patients (5%). Recurrent stroke occurred in 2 patients (1%). Results Two hundred four patients were analyzed. Main Outcome Measures Symptomatic hemorrhagic transformation, stroke progression, and discharge modified Rankin Scale score. Laboratory values were captured from the records. Outcome measures and adverse events were collected prospectively. Patients were grouped by treatment: no treatment, aspirin only, aspirin followed by warfarin sodium, intravenous heparin sodium in the acute phase followed by warfarin (heparin bridging), and full-dose enoxaparin sodium combined with warfarin (enoxaparin bridging).

Still, uncertainty exists regarding the best mode of starting long-term anticoagulation.ĭesign, Setting, and Patients We conducted a retrospective review of all patients with cardioembolic stroke admitted to our center from April 1, 2004, to June 30, 2006, and not treated with tissue plasminogen activator. Shared Decision Making and Communicationīackground Most patients with cardioembolic stroke require long-term anticoagulation.
Scientific Discovery and the Future of Medicine.Health Care Economics, Insurance, Payment.Clinical Implications of Basic Neuroscience.Challenges in Clinical Electrocardiography.


 0 kommentar(er)
0 kommentar(er)
